



Microvascular decompression (MVD) is a neurosurgical procedure used to relieve abnormal compression of a cranial nerve by a nearby blood vessel. This compression can cause chronic nerve pain, muscle spasms, or loss of function.

Targets the trigeminal nerve (responsible for facial sensation).
Treats severe facial pain caused by nerve compression.
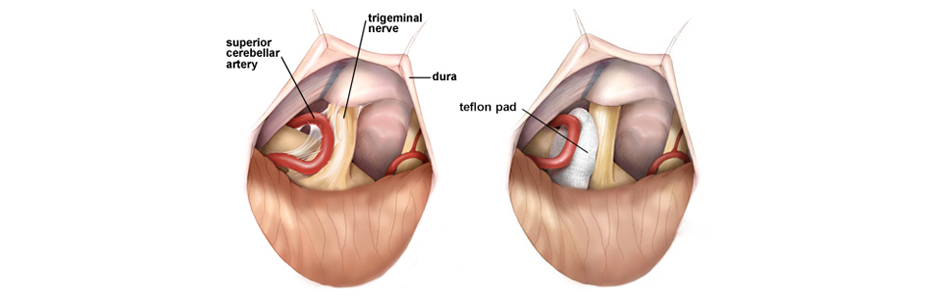
Involves repositioning or separating the compressing blood vessel.

Targets the facial nerve.
Treats uncontrollable facial muscle spasms.
The surgeon places a Teflon pad between the nerve and blood vessel.

Targets the glossopharyngeal nerve.
Treats throat and ear pain caused by compression.
Involves separating or cushioning the compressing vessel.
MVD is typically performed when patients experience:
Severe facial pain on one side.
Electric-shock-like or stabbing sensations.
Pain triggered by touch, chewing, or brushing teeth.
Uncontrollable facial twitching or spasms.
Spasms begin around the eye and spread across the face.
Gradual worsening of spasms over time.
Sharp, stabbing pain in the throat, tonsils, or ear.
Triggered by swallowing, talking, or coughing.
Episodes of intense pain lasting seconds to minutes.
While MVD is generally safe, certain factors may increase the risk of complications:

MVD is performed when nerves are compressed by surrounding blood vessels, leading to chronic pain or spasms:
An artery or vein presses against the nerve.
This causes irritation and misfiring of nerve signals.
Common in trigeminal neuralgia and hemifacial spasm.
As blood vessels harden with age, they can compress nearby nerves.
This leads to progressive nerve dysfunction.
Brain tumors or cysts can press on cranial nerves.
Causes chronic pain or muscle spasms.
Structural abnormalities can result in nerve compression.
May require MVD to relieve the pressure.
While MVD is a treatment, not a condition, you can reduce the risk of nerve compression conditions through:
Control hypertension and cholesterol to prevent vessel enlargement.
Avoid excessive alcohol and smoking.
For patients with chronic nerve conditions, regular monitoring can detect early symptoms.
Use nerve pain medications as prescribed.
Early treatment with medications may reduce the need for surgery.
Helps manage muscle spasms and improves nerve function.
Reduces dependence on surgical intervention.
Before considering MVD, doctors may recommend non-surgical treatments:
Anticonvulsants (carbamazepine, gabapentin) to reduce nerve pain.
Muscle relaxants (baclofen) for spasms.
Pain relievers (NSAIDs or opioids) for temporary relief.
Used for hemifacial spasms.
Temporarily reduces muscle contractions.
May require repeat injections every 3–6 months.
Non-invasive radiation treatment.
Targets the compressed nerve, reducing pain.
Less effective for severe cases.
Local anesthetic injections near the affected nerve.
Provides temporary pain relief.


Performed under general anesthesia.
A small opening is made in the skull behind the ear.
The surgeon repositions or cushions the blood vessel compressing the nerve.
Teflon pads may be placed between the vessel and nerve.
Hospital stay: 2–5 days.
Recovery time: 4–6 weeks.

Minimally invasive approach.
Uses a small camera and specialized instruments.
Requires smaller skull opening.
Faster recovery and fewer complications.

Utilizes MRI or CT guidance during surgery.
Increases precision and reduces complications.
Preferred for complex cases.

2–5 days, depending on the procedure.
4 – 8 weeks, with gradual improvement.
Avoid heavy lifting and strenuous activity.
Take prescribed pain medications.
Attend follow-up appointments.

High success rate (over 80%) for trigeminal neuralgia and hemifacial spasm.
Long-lasting pain relief.
Improves quality of life.
Minimally invasive with low recurrence rates.